Surgical style masks are not designed to protect the wearer… respirators are.
Masks vs Respirators what’s the Difference?

Respirator Standards
The US Center for Disease Control (CDC) cites the N95 respirator standard as part of the advised protective equipment in their Covid-19 FAQ and their SARS guidance (SARS being a similar type of Corona virus). Which suggests that an N95 or better respirator is acceptable.
N95 vs FFP3 & FFP2
The most commonly discussed respirator type is N95. This is an American standard managed by NIOSH – part of the Center for Disease Control (CDC).
Europe uses two different standards. The “filtering face piece” score (FFP) comes from EN standard 149:2001. Then EN 143 standard covers P1/P2/P3 ratings. Both standards are maintained by CEN (European Committee for Standardization).

| Respirator Standard | Filter Capacity (removes x% of of all particles that are 0.3 microns in diameter or larger) |
|---|---|
| FFP1 & P1 | At least 80% |
| FFP2 & P2 | At least 94% |
| N95 | At least 95% |
| N99 & FFP3 | At least 99% |
| P3 | At least 99.95% |
| N100 | At least 99.97% |
The closest European equivalent to N95 are FFP2 / P2 rated respirators, which are rated at 94%, compared to the 95% of N95. Similarly, the closest to N100 are P3 rated respirators – with FFP3 following closely behind.
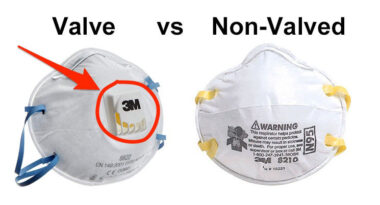
Valve vs Non-Valved Respirators
Valved respirators make it quicker and easier to exhale air than their non-valved counterparts. This makes them more comfortable to wear, and leads to less moisture build-up inside the respirator. This is particularly useful with the higher rated filters (N100/FFP3), which require more force to exhale through.
One important caveat is that valved respirators may not be optimal in settings where you want to stop the wearer from spreading infection. If the wearer is ill, the valve will mean that their out breath / coughs / sneezes will make their way through the mask, and into the air, without filtering. This is due to the valve opening when exhaling.
How big is the Coronavirus, and can respirators filter it?
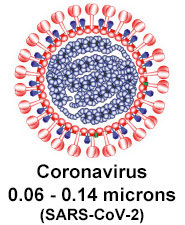
YES! Respirators with high efficiency at 0.3 micron particle size (N95/FFP2 or better) can filter particles down to the size of the coronavirus (which is around 0.1 microns).
A recent paper shows that the coronavirus ranges from between 0.06 and 0.14 microns in size. Note that the paper refers to the coronavirus particle as 2019-nCoV, which was its old name. The virus is currently called 2019-CoV-2, and the illness it presents in people is called Covid-19
What are respirators protecting us against?
Droplets: A primary reason for wearing a respirator is to protect from droplets. For example if a sick person coughs or sneezes when in close proximity to us, the respirator forms a barrier to prevent their bodily fluids reaching our face.
Droplets are large, and gravity drags them down to land on objects, rather than staying in the air. So they don’t travel very long distances
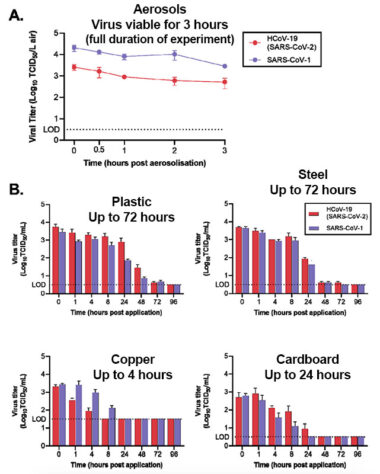
Aerosols: What may remain in the air for some time are aerosolized virus particles. So for example, you could imagine someone creating two issues when sneezing, the first are ejected droplets, which travel a short distance, then second, aerosolized virus particles that stay in the air for longer.
Currently there is debate and uncertainty around how long Covid-19 can remain aerosolized, and how much of a risk that vector is, compared to others.
What we can do is be aware of what research currently says, and err on the side of caution until it has been confirmed.
Scientists at the National Institute of Allergy and Infectious Diseases (NIAID) examined what can happen under controlled lab conditions (link to study). They used a nebulizer, which creates an aerosol from liquids, and tested how long the virus remains viable in the air whilst aerosolized. They also tested how long the virus lasts on other surfaces. Their results showed the virus remained viable for the full duration of the aerosolization experiment; 3 hours. See the graphs below for more details:
Can Surgical Masks Filter the Coronavirus?

Surgical masks are primarily designed to protect vulnerable patients from medical professionals. Stopping the wearer (e.g. surgeon) from spreading their germs when coughing/sneezing/speaking. They are designed to protect patients, not to protect the wearer.
An obvious flaw with surgical masks compared to respirators is their lack of a tight face fit, which leaves gaps around the edges. There is not currently research available on the efficacy of surgical masks (or even respirators), for protecting wearers against the coronavirus. This isn’t surprising given how new the virus is.
In lieu of that, Let’s look at research around the use of surgical masks and N95 masks in the context of influenza, looking specifically at the protection given to the wearers. Influenza may be a good virus particle to compare it to, as they are both transmissible through droplets and aerosol, both cause respiratory infection, and both are similar in particle size.
Please don’t conflate the comparison to the influenza particle as suggestion that they are comparable illnesses – current data suggests that the coronavirus may have a higher mortality rate.
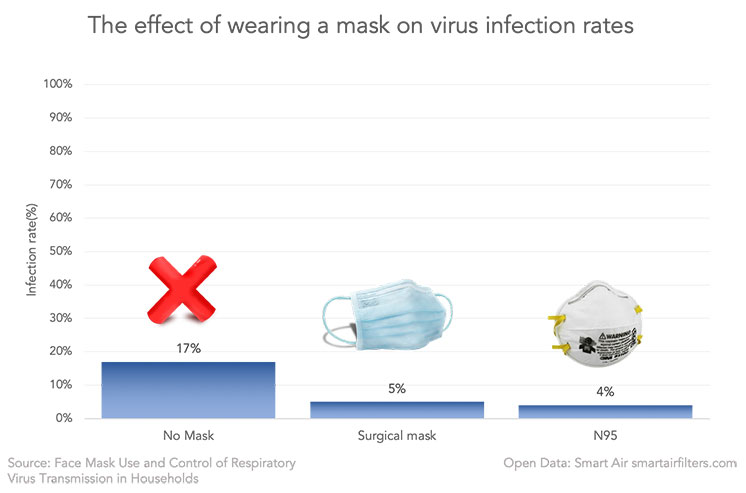
- Wearing a surgical mask or N95 (FFP2) respirator was better (in the study) at protecting against influenza-like illnesses than wearing nothing at all
- Whilst we can anticipate surgical masks to be inferior to respirators, the studies above suggest they are not as inferior as one might assume. For example, the first two studies didn’t find a significant difference between surgical masks and N95 respirators, when protecting wearers against influenza.
- Important to note that we’ve used influenza protection as a proxy for SARS-CoV-2 (coronavirus). This is done because SARS-CoV-2 is new and there are no comparable studies on it. However, of course the drawback is that it still leaves a lot of uncertainty, as SARS-CoV-2 may act quite differently in terms of transmission.
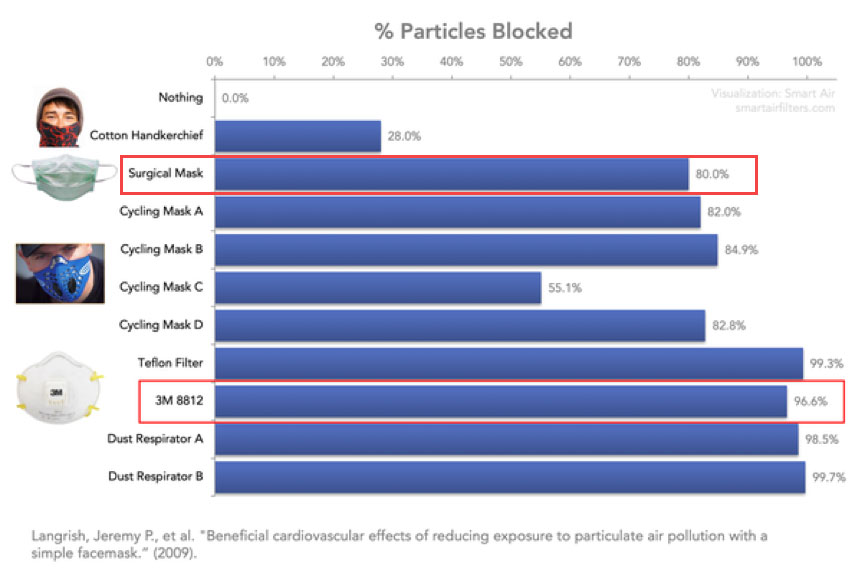
In a lab setting, with artificial conditions, we find that surgical masks are able to block 80% of particles down to 0.007 microns as compared to the 3M 8812 respirator, in this study, which blocked 96% (FFP1 rated). This generally aligns with our discussion above.
In conclusion:
we don’t know how much protection surgical masks provide against the novel coronavirus. However, the above at least suggests that a surgical mask may provide more than zero protection. It makes sense to wear them for protection as a method of last resort – with respirators being the primary choice.
